Understanding Hysterectomy: What It Means & What to Expect


Facing a hysterectomy can bring a host of questions and concerns. This procedure, which involves removing the uterus, is often the recourse for persistent conditions like severe endometriosis, symptomatic fibroids, chronic pelvic pain, prolapse, or cancer. This guide provides an overview of the surgical procedure, detailing the types, the healing process, and adjustments that come afterward, to offer clarity and prepare you for the next steps on your health journey.
Key Takeaways
A hysterectomy is a surgical procedure to remove the uterus typically performed as a last resort when other treatments fail, and it may be essential for conditions like painful uterine fibroids and severe endometriosis.
Different types of hysterectomy include total, supracervical, and radical (including ovaries and surrounding lymph nodes), with the choice of the procedure depending on the medical condition; minimally invasive methods like laparoscopic or robotic hysterectomies are also available.
Postoperative recovery from a hysterectomy requires several weeks, with potential complications such as infection and bleeding; emotional support and treatment options are important for dealing with the physical and hormonal changes following surgery.
An Introduction to Understanding Hysterectomy
A hysterectomy is a surgical procedure that removes the uterus. In some cases, it may also involve taking out the cervix, ovaries, or fallopian tubes. This surgery is often done to treat conditions like fibroids, endometriosis, or cancer, but it can also be necessary for chronic pain or excessive bleeding that doesn’t respond to other treatments. Knowing what to expect before, during, and after the procedure can help ease worries and prepare you for the journey ahead.
Moreover, certain conditions such as uterine fibroids, prolapse, severe endometriosis, and heavy vaginal bleeding may necessitate a hysterectomy. Lesser procedures such as a supracervical hysterectomy, which maintains the pelvic structures and cervix, helps to allow continued vaginal sexual function. But don’t let the thought of a hysterectomy scare you. After all, understanding the why behind the procedure is the first step toward preparation.
The Spectrum of Hysterectomy Types
As we get into. more detail, it’s important to note that not all hysterectomies are created equal. The types of hysterectomy performed largely depend on the extent of organ removal involved. From total to supracervical and radical, each type offers varying levels of organ removal tailored to specific medical conditions. In addition, advancements in medical technology have given rise to minimally invasive methods such as vaginal or laparoscopic hysterectomy, laparoscopically assisted vaginal hysterectomy, and laparoscopic or robotic hysterectomy, providing alternatives to traditional methods.
Let’s take a look at these types.
Total Hysterectomy
Of the different types of hysterectomies, the total hysterectomy is quite common. As the name suggests, this procedure involves the surgical removal of both the uterus and the cervix, either through the vagina or an abdominal incision. This means that the entire uterus, along with the cervix, is removed during the procedure.
Interestingly, despite the significant removal, the ovaries and fallopian tubes aren’t typically removed in a total hysterectomy for non-cancerous conditions. This makes the procedure the most common form of hysterectomy. It’s a process that requires precision and careful execution, but with the right Gynecological team, it’s a manageable procedure.
Supracervical Hysterectomy
A supracervical hysterectomy, also known as a partial or subtotal hysterectomy, differs slightly from a total hysterectomy. In this procedure, only the upper portion of the uterus is removed, leaving the cervix intact. This means that while the uterus is removed, the cervix remains, offering a unique approach to hysterectomy that may be preferable for certain medical conditions or personal reasons. For instance, some women may choose to keep their cervix in place if they believe it will help maintain pelvic floor support or reduce the risk of vaginal prolapse. Additionally, retaining the cervix may have implications for sexual function, as some believe it can help preserve sexual sensation. However, it's important to note that the medical community is still debating these potential benefits, and the decision should be made in consultation with a Gynecologist, considering the individual's specific circumstances and health goals.
One thing to note, with the cervix remaining, it’s important to remember that regular Pap tests are necessary for cervical screening. This ensures that any potential issues are caught early, prioritizing your health and wellbeing.
Radical Hysterectomy
The most comprehensive of the bunch, a radical hysterectomy involves the removal of pelvic organs and structures, including:
the uterus
the cervix
the upper vagina, which is sometimes involved in a vaginal hysterectomy
surrounding tissue of the cervix
sometimes the pelvic lymph nodes
ovaries and fallopian tubes
This procedure is typically performed as a treatment for cancer, targeting the disease at its root.
The radical nature of this procedure, which sometimes involves dealing with scar tissue, shows the lengths that medical professionals go to in ensuring your health. It’s radical, yes, but sometimes, it’s necessary.
The Journey Through Hysterectomy Surgery
Having explored the types of hysterectomies, let’s now discuss the actual procedure. It all begins with general anesthesia to ensure you’re unconscious and pain-free during the surgery. Prior to the surgical incision, the abdomen, and vaginal canal are cleaned with a sterilizing solution. The operative space is then expanded for better visualization once the abdomen is opened.
The process involves several precise steps, including:
Ligating and dividing the round ligament to facilitate the removal of the uterus
Clamping, cutting, and ligating the uterine artery and vein to detach the uterus from its blood supply
Suturing the vaginal cuff closed to ensure there are no bleeding concerns
Undergoing major surgery, which typically lasts between one to two hours, marks the beginning of the journey to recovery.
Pre-Op Preparation
There are specific guidelines to prepare for a hysterectomy, including do’s and don’ts that your healthcare team will walk you through. These guidelines are designed to ensure your body is in the best possible condition for the surgery and to minimize the risk of complications. You may be advised to stop taking certain medications, such as blood thinners, to reduce the risk of excessive bleeding. It’s also common to be asked to fast for a certain period before the surgery to prevent anesthesia-related complications. Your healthcare provider will likely recommend that you arrange for assistance at home during your initial recovery period, as your mobility and physical capabilities will be limited. Additionally, you may be asked to perform specific exercises or follow a particular diet to enhance your recovery post-surgery. Light exercise and avoiding prolonged sitting are crucial to reduce the risk of blood clots and deep vein thrombosis. Adhering strictly to these instructions is crucial for a successful surgery and a smooth recovery.
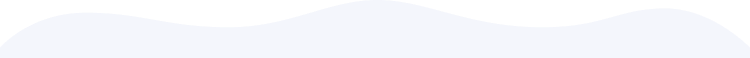
Resources are available to help you get ready for the surgery. One such resource is a structured framework such as Ready Set Recover, designed to help you prepare both physically and mentally for the procedure. Preparation is about more than just the physical aspect; it’s also about ensuring that you’re mentally ready for what lies ahead. Additionally, online support groups and forums can provide a community of individuals who have gone through similar experiences, offering emotional support and practical advice. Educational materials from reputable medical institutions and personalized checklists for pre- and post-surgery preparations can also be invaluable resources. It’s essential to utilize a combination of these tools to be as informed and comfortable as possible with the process.
Post-Op Expectations: Healing and Complications
Post-surgery, it’s important to know what to expect. Recovery from an abdominal hysterectomy generally spans several weeks, with patients spending a short period in a hospital before continuing recovery at home. During this period, patients are advised to rest, avoid heavy lifting, avoid constipation, and gradually reintroduce activities over six to eight weeks.
However, the journey isn’t always smooth. Complications can arise, including:
Fever-Inadequate breathing
Chills-Infection
Vaginal bleeding
Severe pain
Problems with urination or bowel movements
Injury to a ureter
Additionally, patients should monitor for post-operative symptoms such as vaginal discharge.
It’s important to keep an open line of communication with your healthcare team to promptly address any concerns and ensure a smooth recovery.
Life After Uterus Removal: Physical and Emotional Adjustments
Life after a hysterectomy brings about a slew of physical and emotional adjustments. If the ovaries have been removed, menopausal symptoms can occur immediately, resulting in hormonal adjustments or early onset of menopause. This can cause a range of changes, including:
Sleep disturbances
Mood swings
Hot flashes
Vaginal dryness
Decreased libido
Weight gain
It’s important to talk to your doctor about managing these symptoms and finding the best treatment options for you.
Additionally, protecting and strengthening pelvic floor muscles is crucial to support healing tissues and encourage normal bowel and bladder function. This can help reduce strain on the pelvic floor muscles during recovery.
Moreover, many women experience an emotional upheaval after a hysterectomy. Feelings of sadness, loss, or a shift in their sense of feminine identity may occur. Support from loved ones, support groups, or professional therapy can help facilitate emotional recovery. Remember, it’s normal to experience these emotions and seek help when needed.
Navigating Menopause Symptoms Post-Hysterectomy
Navigating the tides of menopause post-hysterectomy can be challenging, especially for those who have undergone the procedure due to ovarian cancer.
Treatment options are available to manage these symptoms. Non-hormonal treatments, including antidepressants and seizure medications, may be used to alleviate symptoms. Hormone replacement therapy (HRT) is also commonly recommended, with the suggestion to continue HRT until the average age of natural menopause.
It's a bit of a journey, but with the right advice by your side, you'll totally be able to handle it. Learn more about depression after surgery and some potential coping strategies.
Alternatives to Hysterectomy: Exploring Other Treatments
A hysterectomy isn’t the only solution to conditions that affect the uterus, such as uterine prolapse. Hormonal management using estrogen or progesterone offers an alternative for controlling bleeding. Additionally, procedures like endometrial ablation, which destroys the uterine lining, can serve as a less invasive option for women not planning future pregnancies.
Other alternatives include uterine artery embolization, a non-surgical procedure that impedes the blood supply to uterine fibroids. Myomectomy, a surgery that removes only the fibroids while preserving the uterus, is suitable for women who wish to maintain fertility. It’s all about finding the right path for you, and sometimes, it’s not a hysterectomy.
Hysterectomy Recovery Timeline and Tips
Understanding the recovery timeline can help you plan and prepare for life post-hysterectomy. Full recovery from an abdominal hysterectomy can take approximately 6 to 8 weeks, while recovery times for vaginal or laparoscopic hysterectomies are generally shorter.
While recovering, patients are encouraged to avoid heavy lifting and ensure adequate rest to facilitate the healing of the abdominal muscles and surrounding tissues. Returning to normal activities can vary from 2 to 8 weeks, depending on the individual’s recovery and the nature of their daily tasks. Remember, each body heals at its own pace, and it’s important to listen to yours.
Sexual Health After Hysterectomy
The impact of a hysterectomy on sexual function is a topic that deserves attention. Relief from pre-surgery symptoms such as bleeding and pain may improve overall sexual satisfaction post-hysterectomy. Research indicates that there is generally no significant change in overall sexual function following a hysterectomy.
However, some women might experience pain during sexual intercourse post-hysterectomy. Here are some strategies that can help alleviate this pain:
Using different sexual positions
Using lubricants
Using low-dose vaginal estrogen
Pelvic floor physical therapy can also be beneficial for recovering muscle tone and control, thus helping to alleviate pain during intercourse.
Maintaining Health with Regular Screenings
After a hysterectomy, maintaining health through regular screenings is crucial. Regular Pap tests may still be needed to screen for cervical cancer, depending on individual health circumstances. Individuals with prenatal exposure to diethylstilbestrol (DES) should have regular Pap tests due to an increased risk of cervical cancer.
Routine Pap test screening is typically considered unnecessary after age 65 if there is a history of normal results and no high risk for cervical cancer. However, it’s always best to discuss this with your health care team to ensure you’re on the right path for maintaining your health.
A New Chapter: Understanding Hysterectomy and Embracing Wellness
Starting the journey of a hysterectomy can feel intimidating, but with the right knowledge and support, it turns into something you can handle. We’ve explored the reasons behind a hysterectomy, different types, and the recovery process. We’ve also touched on life after surgery, the menopause symptoms that may arise, and alternative treatments. Remember, it’s your body, your health, and you have the right to understand every aspect of it. Embrace the journey, and remember, you’re not alone.
Frequently Asked Questions
How painful is a hysterectomy?
A hysterectomy can involve post-operative pain and tiredness for a few weeks, but during the surgery, you will be under general anesthesia and will not feel any pain. The procedure typically takes 1 to 2 hours.
How long does it take to recover from hysterectomy?
The recovery time for a hysterectomy varies depending on the type of operation and your overall health, typically ranging from 3 to 6 weeks.
What is life like after hysterectomy?
After a hysterectomy, you may experience changes in your hormones, such as the onset of menopause symptoms and a decrease in sexual desire. Your body will need time to adjust to the new hormone levels and you may experience symptoms like hot flashes and mood swings.
What happens to a woman when she’s had a hysterectomy?
After a hysterectomy, a woman will no longer have periods, can no longer have children, and may experience menopause symptoms if the ovaries are removed. This can include vaginal dryness, hot flashes, and reduced interest in sex.
What are the common reasons for a hysterectomy?
Common reasons for a hysterectomy include persistent pelvic pain, uterine fibroids, and severe endometriosis.
How long does it take to heal internally after hysterectomy?
Internal healing usually takes about 6 to 8 weeks, but full recovery depends on the type of hysterectomy and individual health factors.